Overview
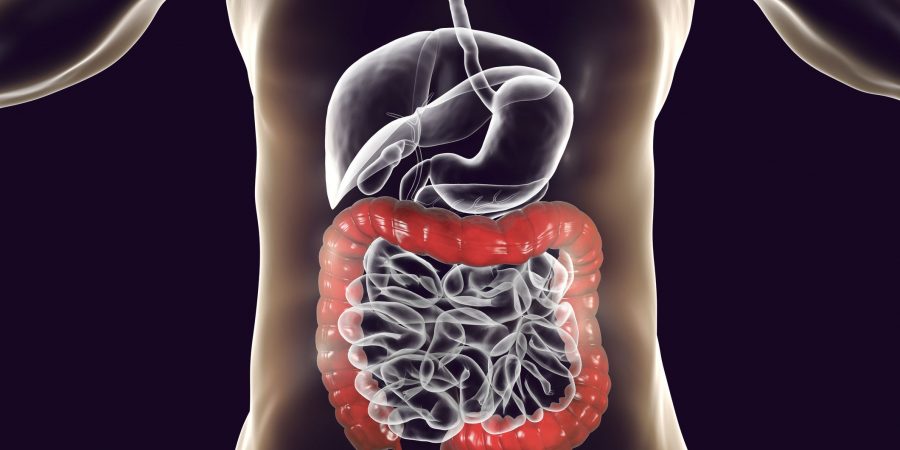
Inflammatory bowel disease (IBD) refers to a group of gastrointestinal disorders driven by chronic inflammation (pain and swelling) in the intestines. IBD includes Crohn’s disease, colitis, microscopic colitis and ulcerative colitis. All types affect the digestive system and are lifelong, with periods of flare and remission.
IBD is commonly diagnosed between the ages of 15-30 years, effecting all genders.
To differentiate:
IBD is a chronic inflammatory disease effecting tissue anywhere between the mouth and anus.
IBS is a gut syndrome classified by a cluster of symptoms of no known cause.
Whilst symptoms can be similar, diagnosis, causes and treatment are very different. IBD is driven by active inflammation and damage to the gut lining, its considered autoimmune and in some cases the patient may require surgery to remove damaged sections of the colon.
Conventional medicine has no cure for IBD but aims to manage severity of symptoms with prescription anti-inflammatories, immunosuppressants and as a last resort surgery.
Causative factors
The exact cause of IBD is subject of much debate. Traditional medicine accepts the following components are involved in IBD development:
- Genetics – family history appears to increase risk
- Immunity – an initial immune response to a pathogen/virus/bacterium within the colon leads to immune confusion and identification of the hosts own colonic tissue as a pathogen. This persistent inappropriate immune response sets up autoimmunity and IBD.
Functional Medicine considers the involvement of Intestinal Permeability as being strongly involved in autoimmune conditions including IBD development, alongside a trigger such as trauma, stress and acute illness.
Symptoms
Abdominal pain, cramps and or swelling
- Gas
- Bloating
- Urgent loose stools – diarrhoea
- Multiple daily bowel movements
- Mucus in stool
- Recurring or bloody diarrhoea
- Weight loss
- Malnutrition
- Extreme tiredness
- Anaemia
- High temperature
- Being sick (vomiting)
- Persistent mouth ulcers (Ulcerative Colitis)
Symptom presentation varies in severity and not all sufferers will experience all symptoms.
Associated Conditions
- SIBO
- Gastrointestinal yeast overgrowth (small and large colon)
- Arthritis
- Concurrent autoimmune conditions
- Lactose Intolera
- Increased Food Sensitivities
- Painful red eyes (uveitis),
- Painful red skin bumps (erythema nodosum)
Functional Tests
The diagnosis of Crohn’s disease or Colitis is made by a Gastroenterologist.
My role is to better understand potential driving factors of your IBD. A deeper dive into the patient’s colonic environment provides insight into best course of action. Understanding alterations in colonic microbiome, bacterial diversity, yeast colonisation, immune and inflammation activity, digestion, faecal fat content and mucosal barrier function provide invaluable information. From this I can build a personalised dietary and lifestyle programme to improve health and symptom management.
Key tests to better understand your IBD include:
- Comprehensive Stool Analysis with or without parasitology
- Small Intestinal Bacterial Overgrowth (SIBO) breath testing
- Lactose Intolerance breath testing
- Organic Acid Testing
- Food Intolerance and Allergy Testing
- Coeliac Disease testing
- Advanced Gut Barrier Assessment and Intestinal Permeability testing (leaky gut)
Intervention Consideration
Specific dietary approaches have been shown to improve IBD symptoms. Through diet and lifestyle intervention the aim is to reduce active inflammation, modulate microbiome and support digestion. Addressing functional test findings allows for bespoke nutrition advice and targeted action.
Therapeutic supplementation may be considered, aimed at addressing nutrient deficiencies commonly associated with IBD, alongside management of gut flora and inflammation.